Case Summary
Warner Chilcott UK complained about the promotion of Octasa (mesalazine modified- release tablets) by Tillotts Pharma UK. The material at issue was a journal supplement published in the British Journal of Clinical Pharmacy. Warner Chilcott marketed Asacol (mesalazine modified release).
The detailed response from Tillotts is given below.
Warner Chilcott submitted that the supplement looked like a non-promotional, educational update – as indicated by its title 'Educational update' – produced by two independent health professionals and formatted in the house style of The British Journal of Clinical Pharmacy. These features were not consistent with a promotional supplement. The Code was explicit on this point and clearly indicated that promotional material in journals should not resemble independent editorial matter.
The Panel noted that Tillotts had provided data and reviewed and approved the article. The supplement was entitled 'Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modifiedrelease mesalazine formulation available?'. Octasa prescribing information was included. The Panel considered that Tillotts was inextricably linked to the production of the supplement.
Further, the company had submitted that it had provided reprints of the supplement to support Octasa, vs Asacol and had cited it in other materials. In the Panel's view, Tillotts was thus responsible under the Code for the content of the supplement. The front cover of the supplement was headed 'Educational update' which was underlined in red. The names of two independent authors appeared in the middle of the front cover. The outside top corner of each page of the article which made up the supplement, featured a red box labeled 'Educational update' in bold white type. A declaration of sponsorship appeared at the bottom of the cover page and again at the end of the article on page 3; the Octasa prescribing information appeared on page 4.
The Panel noted Tillotts' involvement with the material and considered that although there were elements to show that the supplement was a promotional piece, its prominent characterisation as an 'Educational update' was such that the promotional nature of the material was disguised. In this regard, the Panel further noted Warner Chilcott's submission that the supplement was formatted in the house style of the journal. Although the Panel had not been provided with a copy of The British Journal of Clinical Pharmacy, it noted that a paper previously published in the same journal, had a similar three column layout and heading structure. A breach of the Code was ruled.
Warner Chilcott noted that the font size of the declaration of sponsorship statement was disproportionately small and the reader could easily miss it at the foot of the first page. Even if this declaration was read, claims for Octasa had already been made earlier on the page.
The Panel noted that Tillotts' declaration of sponsorship appeared on the front cover of the supplement and again at the end of the article. The declaration on the front cover was at the bottom of the page in small white type (a lower case 'm' was less than 2mm high) on a dark grey background. The dark grey band at the bottom of the page occupied 22% of the cover depth; the declaration of sponsorship statement within that band occupied 5% of the cover depth. The declaration statement was below larger type, on the same dark grey background, which referred to the associated journal. All other text on the cover was similarly in bigger and/or bolder type. The prominence of the heading 'Educational update', the title of the article and the author's names and affiliations was emphasized by the bold white type in which they were written appearing on a black background. The red underlining of 'Educational update' kept the reader's eye to the top or middle of the page. In the Panel's view, the declaration of sponsorship was such that the reader's eye would not be drawn to what appeared to be 'the small print' at the bottom of the page. In that regard the Panel did not consider that the statement was sufficiently prominent to ensure that readers were aware of it at the outset. A breach of the Code was ruled.
The claim 'Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modified-release mesalazine formulation available?' appeared as the title of the supplement and of the article. Warner Chilcott did not accept that the question mark at the end of the title altered the nature of this wording, ie it was a claim for Octasa MR. Although no direct attempt to substantiate this claim was made, the reader was introduced in the first paragraph of the article to a list of seven available modified-release mesalazine products. No cost data were presented yet the title implied that Octasa was the cheapest option.
However, even if taking a cost minimisation approach, which might be questionable with no head-to-head clinical data for any of these products vs Octasa, the acquisition cost of mesalazine therapy should also take into consideration the prescribed daily dosage of mesalazine which varied by product and indication. Using the recommended dosing schedules and the prices presented in MIMS, May 2013, it was clear that there were mesalazine products/doses available in the UK with a lower acquisition cost than some daily doses of Octasa, including pH-dependent, modified release tablets.
Furthermore, this claim implied that both Octasa preparations were equivalently priced, which was not so; the daily cost of 2.4g/day mesalazine was greater for Octasa MR 800mg tablets than for Octasa MR 400mg tablets. Clearly both Octasa products could not be the lowest cost formulation available as one was more expensive than the other. Thus, to make a broad claim that Octasa MR was the lowest cost, oral, pH-dependent, modified-release mesalazine formulation available was inaccurate, misleading and incapable of substantiation.
In the Panel's view, although the title was presented as a question, readers would assume it was a claim ie that Octasa MR was the lowest cost, oral, pHdependent, modified-release mesalazine available.
The first paragraph of the article introduced the reader to the seven modified-release mesalazine preparations which were available until the end of 2012. In that regard the Panel considered that the claim would be seen in the context of these seven medicines ie that Octasa was the lowest cost compared with them all. The Panel noted that additional data provided by Tillotts showed that Octasa MR 400mg tablets (2.4g/day) was the least expensive treatment option for acute treatment. However, for maintenance therapy a dose of Salofalk 1.5g was the least expensive option and Pentasa sachets were also less expensive than Octasa given that the highest maintenance dose of Octasa was 2.4g/day.
The Panel considered that the basis of the claim at issue had not been made abundantly clear. It was not clear as to which doses were included and if the claim related to acute treatment, maintenance treatment or both. The Panel considered that the claim was misleading as alleged and it could not be substantiated; breaches of the Code were ruled.
Warner Chilcott noted the statement 'This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care' appeared as part of the sub-heading to page 1 of the article. Warner Chilcott stated that in its view, the article neither presented nor referred to any evidence or data relating to the clinical benefits of Octasa in patient care. The supplement discussed the in vitro dissolution characteristics and cost differences between Asacol MR 400mg/800mg tablets and Octasa (Mesren) MR 400mg/800mg tablets. It appeared therefore that the statement 'without compromising patient care' was based purely on the extrapolation of in vitro data to the clinical situation and implied that without clinical evidence, interchanging the products discussed would not affect patient management or compromise patient care. To make this assumption without clinical data to show that it was of direct relevance and significance was misleading, in breach of the Code.
The Panel noted that the statement at issue was the second sentence to the subheading on page 1 of the article. The sub-heading, in full, read:
'The discontinuation of Mesren MR (mesalazine' Teva Pharmaceuticals) could have considerable cost implications for the NHS. This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care.'
The Panel noted that with the discontinuation of Mesren, patients previously taking that medicine would have to be switched to an alternative mesalazine product. The Panel further noted that Octasa was, as stated in the article, essentially a rebrand of Mesren; the formulation of both medicines was the same. In the Panel's view, patients switching from Mesren to Octasa should not notice a clinical difference in therapy. The Panel considered that in the context of the discontinuation of Mesren MR, the statement at issue was not misleading as alleged. No breach of the Code was ruled.
Warner Chilcott submitted that whilst the supplement referred to the British Society of Gastroenterology (BSG), the European Crohn's and Colitis Organisation (ECCO) and the British National Formulary (BNF) guidelines and statements, it was quick to disregard the caution represented by these bodies in relation to indiscriminate switching between mesalazine brands and the recommendation to prescribe modified-release mesalazine by brand. To date, there had been no head-to-head clinical studies between Octasa and any other mesalazine and very few head-to-head clinical studies between the different modifiedrelease mesalazines in general. Absence of evidence showing clinical differences between mesalazines (because these studies had not been conducted) was not equivalent to evidence demonstrating no clinically significant differences between the mesalazines, hence the caution in the guidelines that these products should not be considered interchangeable. Dismissal of these cautions and recommendations supported Tillotts' aim to have mesalazine patients indiscriminately switched to Octasa and misrepresented the guidelines in this way was misleading and did not encourage the rational use of Octasa.
Furthermore, Warner Chilcott noted the comment that the BNF statement was 'originally made before the introduction of Mesren MR 400mg and Octasa MR 400mg to the UK market'. Whilst that might or might not be true (Mesren MR 400mg tablets were first licensed in the UK in November 2003) the comment implied that the BNF's position was outdated and could be further disregarded on these grounds. Warner Chilcott noted that the BNF was updated regularly and as it continued to use this statement, it presumably reflected the BNF's current position and was not an outdated recommendation as implied. Warner Chilcott alleged that this section of the supplement misled by distortion and failed to encourage the rational use of Octasa.
The Panel noted that the first section of the journal supplement introduced the reader to seven modified release mesalazine preparations and then stated that the article would describe someof the similarities and differences of three of them – Mesren, Octasa and Asacol. The next section of the article referred to prescribing guidelines and that the BSG and ECCO had recommended that modified-release mesalazine should be prescribed by brand. It was stated however, that both guidelines appeared to suggest that there was little in the way of significant differences between available products with regard to important clinical outcomes. It was noted that the BNF statement which advised that oral mesalazine preparations should not be considered interchangeable was made before Mesren and Octasa had been introduced to the UK market.
The Panel considered that overall, the take home message was that it was not important to prescribe any modified-release mesalazine by brand and that they were all essentially interchangeable. In that regard the Panel noted that the sub-heading referred to 'modified release mesalazine' and so it appeared that the subsequent discussion was not restricted in its scope to Asacol, Mesren and Octasa. The Panel considered that this was misleading. A breach of the Code was ruled.
The Panel did not consider that the information encouraged the rational use of Octasa. A breach of the Code was ruled. Warner Chilcott noted the paragraph entitled 'Are there any significant differences between Asacol MR and Octasa MR?' despite an acknowledgement in the supplement that there was no comparative clinical data for Octasa vs Asacol MR. Instead, the article focussed on data from in vitro dissolution studies to make a case for (clinical) similarity between Asacol and Octasa. However, the methodology of these in vitro studies made it impossible to draw any meaningful conclusions about the similarities or differences between these products in vivo, let alone in various stages of disease activity in patients with ulcerative colitis. Warner Chilcott submitted that in vitro dissolution studies could not fully reproduce the conditions of the gastrointestinal tract in patients with ulcerative colitis. Furthermore, no statistical comparisons between the findings for Mesren and Asacol were presented and no in vitro/in vivo correlation had been established to indicate the potential clinical significance of the findings. Warner Chilcott noted that Fadda and Basit (2005), presented in the supplement, commented on the poor in vitro/in vivo correlations obtained for pH-responsive, modifiedrelease dosage forms. Thus, any conclusions about the significance of the findings of these in vitro data were impossible and attempting to do so in this manner was misleading.
The Panel noted that in the section of the supplement entitled 'Are there any significant differences between Asacol MR and Octasa MR?' it was clearly stated that 'Octasa MR has not been compared directly in a clinical study with Asacol MR'. The Panel considered, however, that most readers would read the rest of the section and assume, even in the acknowledged absence of clinical data, that because the in vitro dissolution characteristics of Mesren and Asacol were similar, the clinical effects of Octasa MR and Asacol MR would also be similar. There was no clinical data toshow that this was so. The Panel considered that the supplement was misleading in this regard. A breach of the Code was ruled.
Warner Chilcott noted that the y-axis of a graph was unlabelled and so it was unclear and ambiguous as to what was presented; it was impossible for the reader to interpret the findings presented. Warner Chilcott alleged that Tillotts had thus failed to maintain high standards in terms of representing the data and reviewing the article before publication.
The Panel noted that the graph was referenced to 'Tillotts Pharma 2012. Data on file' and headed 'Dissolution of Mesren MR 400mg vs Asacol Mr 400mg and 800mg'. The y-axis was not labelled and so in that regard the Panel considered that the graph did not reflect the evidence clearly. The Panel ruled a breach of the Code. The Panel further considered that the use of a poorly labelled graph meant that high standards had not been maintained. A breach of the Code was ruled.
Warner Chilcott alleged that the figure presented for the annual cost of Asacol, 2.4g/day, should be £715.58 and not £715.40 as shown. This error meant that all data derived from this figure was also inaccurate.
Warner Chilcott further submitted that the table was misleading in that it failed to take into account possible changes of dose through a year as patients responded, or not, to therapy. Failure to take this into account in the costs therefore presented an artificial and misleading scenario that would not be encountered in clinical practice and therefore this table presented inflated and unrealistic cost savings that could never be achieved.
Warner Chilcott further submitted that the table failed to state that to obtain the proposed cost savings, the calculations assumed that all 300 patients (the typical number of patients with ulcerative colitis in an average primary care trust (PCT)) would be switched from Asacol to Octasa. This was simply not the case. Although Asacol was the market leader, it had only approximately 40% of market share. As this had not been taken into account, the figures proposed were inflated and misleading.
Other factors omitted from the calculations presented in the table were the cost of implementing such a switch and the management of any relapses or other adverse events. Warner Chilcott was not aware of any clinical study that could be used to accurately describe the true impact of such a switch programme in terms of cost savings or clinical benefit for the patient. However, Robinson et al (2013) demonstrated that stable, adherent patients prescribed Asacol MR formulations had a 3.5 times higher risk of experiencing a flare when switched to another mesalazine product compared with being maintained on Asacol.
The Panel noted that the table at issue compared the daily and annual costs of Octasa MR 400mg, Octasa MR 800mg and Asacol MR all at 2.4g/dayand stated the annual cost savings per patient and per 300 patients if Octasa was prescribed instead of Asacol. The daily cost for Asacol was stated to be £1.96 with an annual cost of £715.40. The Panel noted that data from Tillotts showed that 120 Asacol MR 400mg tablets cost £39.21 ie 196.05 pence per dose of 2.4g which gave an annual cost of £715.58. The Panel noted that the table stated that the annual cost of Asacol 2.4g/day was £715.40 which was not so. The Panel considered that the table was not accurate in that regard as alleged and a breach of the Code was ruled.
The Panel noted that the table stated the annual cost savings per 300 patients if they were prescribed Octasa 2.4g/day instead of Asacol 2.4g/day. The authors had stated that 300 was the typical number of patients for an average PCT, based on a population of 300,000 and an estimated prevalence of ulcerative colitis of between 120 and 150 per 100,000. The Panel noted that this would therefore mean that an average PCT would have 360 to 450 ulcerative colitis patients.
The Panel noted that Tillotts had stated that the prevalence of ulcerative colitis was 240 per 100,000 population and so an average PCT with 350,000 people would have 840 ulcerative colitis patients. Ninety per cent of those patients would be on mesalazine (756) and at least half of them (378) would be on Asacol given its market share.
The Panel thus noted that the authors' justification for assuming 300 patients and Tillotts' justification for the same were quite different. In that regard the Panel considered that the assumptions made in the table were unclear and in that regard the comparisons made within the table were misleading and the data within the table could not be substantiated. Breaches of the Code were ruled.
The Panel noted that Robinson et al post-dated the preparation date of the educational update (December 2012). Robinson et al, however, was a retrospective study using a UK pharmacy dispensing database. Although the authors referred to a 3.5 times greater risk of relapse in adherent patients switched from one mesalazine product to another, compared with non-switch patients, the authors stated that further research was needed before making firm conclusions about the implications of the results for disease management. The Panel noted that there was no clinical data before it which showed that patients switched from one mesalazine to another were more likely to experience a flare in their condition as alleged. On that very narrow basis, the Panel considered that the data in table 1 was not misleading in that regard. No breach of the Code was ruled.
Warner Chilcott noted that the paragraph entitled, 'Are there any cost differences?' essentially summarised the data presented in table 1 and included claims that 'Asacol MR is 50% more expensive than Mesren/Octasa MR 400mg and 25% more expensive than Octasa MR 800mg' and that 'One year of maintenance therapy (2.4g daily) would equate to a £72,000 difference in expenditure for 300 patients'. For all the reasonsdiscussed above Warner Chilcott alleged that these claims were misleading, presented inaccurate and inappropriate cost comparisons and were incapable of substantiation.
The Panel noted that the section of the educational update at issue was a description and justification of the data used in the table considered above. Readers were referred to the table. The Panel noted its comments and rulings above and considered that they applied to the paragraph now at issue. Breaches of the Code were ruled.
Warner Chilcott noted that the concluding paragraph of the supplement contained the claim that 'Octasa MR… represents the least expensive, pH-dependent, modified-release mesalazine product available in the UK'. As indicated above, even with a cost minimisation approach, which might be questionable with no head-to-head clinical data for any mesalazine vs Octasa, claims about the acquisition cost of mesalazine therapy should take into consideration the daily mesalazine dosage which varied by product and indication. Using the recommended dosing schedules and the prices presented in MIMS it was clear that there were mesalazine products/doses available in the UK with a lower acquisition cost than some daily doses of Octasa, including pH-dependent, modifiedrelease tablets. Thus, this claim was alleged to be inaccurate, misleading and incapable of substantiation.
The Panel noted its comments above and considered that they applied here. Breaches of the Code were ruled.
Warner Chilcott submitted that Tillotts' close involvement in the writing, review and approval of this item and in the provision of data to the authors should have assured that the highest standards of content would be maintained. Instead there were a number of fundamental inaccuracies and breaches of the Code which collectively reflected failure to maintain high standards.
The Panel noted its rulings above of breaches of the Code and considered that high standards had not been maintained. A breach of the Code was ruled.
Warner Chilcott was concerned that the multiplicity of fundamental errors and breaches of the Code contained within the supplement potentially put ulcerative colitis patients at risk. A breach of Clause 2 was alleged. The Panel noted its rulings above and that some of the matters considered overlapped. Although concerned about the poor standard of the material at issue, the Panel did not consider that it was such as to bring discredit upon, or reduce confidence in, the industry. No breach of Clause 2 was ruled.
CASE AUTH/2610/6/13 WARNER CHILCOTT v TILLOTTS
Disguised promotion of Octasa in educational supplement
Warner Chilcott UK complained about the promotion of Octasa (mesalazine modified- release tablets) by Tillotts Pharma UK. The material at issue was a journal supplement published in the British Journal of Clinical Pharmacy. Warner Chilcott marketed Asacol (mesalazine modified release).
The detailed response from Tillotts is given below.
Warner Chilcott submitted that the supplement looked like a non-promotional, educational update – as indicated by its title ‘Educational update’ – produced by two independent health professionals and formatted in the house style of The British Journal of Clinical Pharmacy. These features were not consistent with a promotional supplement. The Code was explicit on this point and clearly indicated that promotional material in journals should not resemble independent editorial matter.
The Panel noted that Tillotts had provided data and reviewed and approved the article. The supplement was entitled ‘Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modifiedrelease mesalazine formulation available?’. Octasa prescribing information was included. The Panel considered that Tillotts was inextricably linked to the production of the supplement. Further, the company had submitted that it had provided reprints of the supplement to support Octasa, vs Asacol and had cited it in other materials. In the Panel’s view, Tillotts was thus responsible under the Code for the content of the supplement.
The front cover of the supplement was headed ‘Educational update’ which was underlined in red. The names of two independent authors appeared in the middle of the front cover. The outside top corner of each page of the article which made up the supplement, featured a red box labeled ‘Educational update’ in bold white type. A declaration of sponsorship appeared at the bottom of the cover page and again at the end of the article on page 3; the Octasa prescribing information appeared on page 4.
The Panel noted Tillotts’ involvement with the material and considered that although there were elements to show that the supplement was a promotional piece, its prominent characterisation as an ‘Educational update’ was such that the promotional nature of the material was disguised. In this regard, the Panel further noted Warner Chilcott’s submission that the supplement was formatted in the house style of the journal. Although the Panel had not been provided with a copy of The British Journal of Clinical Pharmacy, it noted that a paper previously published in the same journal, had a similar three column layout and heading structure. A breach of the Code was ruled.
Warner Chilcott noted that the font size of the declaration of sponsorship statement was disproportionately small and the reader could easily miss it at the foot of the first page. Even if this declaration was read, claims for Octasa had already been made earlier on the page.
The Panel noted that Tillotts’ declaration of sponsorship appeared on the front cover of the supplement and again at the end of the article. The declaration on the front cover was at the bottom of the page in small white type (a lower case ‘m’ was less than 2mm high) on a dark grey background. The dark grey band at the bottom of the page occupied 22% of the cover depth; the declaration of sponsorship statement within that band occupied 5% of the cover depth. The declaration statement was below larger type, on the same dark grey background, which referred to the associated journal. All other text on the cover was similarly in bigger and/or bolder type. The prominence of the heading ‘Educational update’, the title of the article and the author’s names and affiliations was emphasized by the bold white type in which they were written appearing on a black background. The red underlining of ‘Educational update’ kept the reader’s eye to the top or middle of the page. In the Panel’s view, the declaration of sponsorship was such that the reader’s eye would not be drawn to what appeared to be ‘the small print’ at the bottom of the page. In that regard the Panel did not consider that the statement was sufficiently prominent to ensure that readers were aware of it at the outset. A breach of the Code was ruled.
The claim ‘Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modified-release mesalazine formulation available?’ appeared as the title of the supplement and of the article. Warner Chilcott did not accept that the question mark at the end of the title altered the nature of this wording, ie it was a claim for Octasa MR. Although no direct attempt to substantiate this claim was made, the reader was introduced in the first paragraph of the article to a list of seven available modified-release mesalazine products. No cost data were presented yet the title implied that Octasa was the cheapest option.
However, even if taking a cost minimisation approach, which might be questionable with no head-to-head clinical data for any of these products vs Octasa, the acquisition cost of mesalazine therapy should also take into consideration the prescribed daily dosage of mesalazine which varied by product and indication. Using the recommended dosing schedules and the prices presented in MIMS, May 2013, it was clear that there were mesalazine products/doses available in the UK with a lower acquisition cost than some daily doses of Octasa, including pH-dependent, modified release tablets.
Furthermore, this claim implied that both Octasa preparations were equivalently priced, which was not so; the daily cost of 2.4g/day mesalazine was greater for Octasa MR 800mg tablets than for Octasa MR 400mg tablets. Clearly both Octasa products could not be the lowest cost formulation available as one was more expensive than the other. Thus, to make a broad claim that Octasa MR was the lowest cost, oral, pH-dependent, modified-release mesalazine formulation available was inaccurate, misleading and incapable of substantiation.
In the Panel’s view, although the title was presented as a question, readers would assume it was a claim ie that Octasa MR was the lowest cost, oral, pHdependent, modified-release mesalazine available.
The first paragraph of the article introduced the reader to the seven modified-release mesalazine preparations which were available until the end of 2012. In that regard the Panel considered that the claim would be seen in the context of these seven medicines ie that Octasa was the lowest cost compared with them all. The Panel noted that additional data provided by Tillotts showed that Octasa MR 400mg tablets (2.4g/day) was the least expensive treatment option for acute treatment. However, for maintenance therapy a dose of Salofalk 1.5g was the least expensive option and Pentasa sachets were also less expensive than Octasa given that the highest maintenance dose of Octasa was 2.4g/day.
The Panel considered that the basis of the claim at issue had not been made abundantly clear. It was not clear as to which doses were included and if the claim related to acute treatment, maintenance treatment or both. The Panel considered that the claim was misleading as alleged and it could not be substantiated; breaches of the Code were ruled.
Warner Chilcott noted the statement ‘This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care’ appeared as part of the sub-heading to page 1 of the article. Warner Chilcott stated that in its view, the article neither presented nor referred to any evidence or data relating to the clinical benefits of Octasa in patient care. The supplement discussed the in vitro dissolution characteristics and cost differences between Asacol MR 400mg/800mg tablets and Octasa (Mesren) MR 400mg/800mg tablets. It appeared therefore that the statement ‘without compromising patient care’ was based purely on the extrapolation of in vitro data to the clinical situation and implied that without clinical evidence, interchanging the products discussed would not affect patient management or compromise patient care. To make this assumption without clinical data to show that it was of direct relevance and significance was misleading, in breach of the Code.
The Panel noted that the statement at issue was the second sentence to the subheading on page 1 of the article. The sub-heading, in full, read:
‘The discontinuation of Mesren MR (mesalazine’ Teva Pharmaceuticals) could have considerable cost implications for the NHS. This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care.’
The Panel noted that with the discontinuation of Mesren, patients previously taking that medicine would have to be switched to an alternative mesalazine product. The Panel further noted that Octasa was, as stated in the article, essentially a rebrand of Mesren; the formulation of both medicines was the same. In the Panel’s view, patients switching from Mesren to Octasa should not notice a clinical difference in therapy. The Panel considered that in the context of the discontinuation of Mesren MR, the statement at issue was not misleading as alleged. No breach of the Code was ruled.
Warner Chilcott submitted that whilst the supplement referred to the British Society of Gastroenterology (BSG), the European Crohn’s and
Colitis Organisation (ECCO) and the British National Formulary (BNF) guidelines and statements, it was quick to disregard the caution represented by these bodies in relation to indiscriminate switching between mesalazine brands and the recommendation to prescribe modified-release mesalazine by brand. To date, there had been no head-to-head clinical studies between Octasa and any other mesalazine and very few head-to-head clinical studies between the different modifiedrelease mesalazines in general. Absence of evidence showing clinical differences between mesalazines (because these studies had not been conducted) was not equivalent to evidence demonstrating no clinically significant differences between the mesalazines, hence the caution in the guidelines that these products should not be considered interchangeable. Dismissal of these cautions and recommendations supported Tillotts’ aim to have mesalazine patients indiscriminately switched to Octasa and misrepresented the guidelines in this way was misleading and did not encourage the rational use of Octasa.
Furthermore, Warner Chilcott noted the comment that the BNF statement was ‘originally made before the introduction of Mesren MR 400mg and Octasa MR 400mg to the UK market’. Whilst that might or might not be true (Mesren MR 400mg tablets were first licensed in the UK in November 2003) the comment implied that the BNF’s position was outdated and could be further disregarded on these grounds. Warner Chilcott noted that the BNF was updated regularly and as it continued to use this statement, it presumably reflected the BNF’s current position and was not an outdated recommendation as implied. Warner Chilcott alleged that this section of the supplement misled by distortion and failed to encourage the rational use of Octasa.
The Panel noted that the first section of the journal supplement introduced the reader to seven modified release mesalazine preparations and then stated that the article would describe some
of the similarities and differences of three of them – Mesren, Octasa and Asacol. The next section of the article referred to prescribing guidelines and that the BSG and ECCO had recommended that modified-release mesalazine should be prescribed by brand. It was stated however, that both guidelines appeared to suggest that there was little in the way of significant differences between available products with regard to important clinical outcomes. It was noted that the BNF statement which advised that oral mesalazine preparations should not be considered interchangeable was made before Mesren and Octasa had been introduced to the UK market.
The Panel considered that overall, the take home message was that it was not important to prescribe any modified-release mesalazine by brand and that they were all essentially interchangeable. In that regard the Panel noted that the sub-heading referred to ‘modified release mesalazine’ and so it appeared that the subsequent discussion was not restricted in its scope to Asacol, Mesren and Octasa. The Panel considered that this was misleading. A breach of the Code was ruled. The Panel did not consider that the information encouraged the rational use of Octasa. A breach of the Code was ruled.
Warner Chilcott noted the paragraph entitled ‘Are there any significant differences between Asacol MR and Octasa MR?’ despite an acknowledgement in the supplement that there was no comparative clinical data for Octasa vs Asacol MR. Instead, the article focussed on data from in vitro dissolution studies to make a case for (clinical) similarity between Asacol and Octasa. However, the methodology of these in vitro studies made it impossible to draw any meaningful conclusions about the similarities or differences between these products in vivo, let alone in various stages of disease activity in patients with ulcerative colitis. Warner Chilcott submitted that in vitro dissolution studies could not fully reproduce the conditions of the gastrointestinal tract in patients with ulcerative colitis. Furthermore, no statistical comparisons between the findings for Mesren and Asacol were presented and no in vitro/in vivo correlation had been established to indicate the potential clinical significance of the findings. Warner Chilcott noted that Fadda and Basit (2005), presented in the supplement, commented on the poor in vitro/in vivo correlations obtained for pH-responsive, modifiedrelease dosage forms. Thus, any conclusions about the significance of the findings of these in vitro data were impossible and attempting to do so in this manner was misleading.
The Panel noted that in the section of the supplement entitled ‘Are there any significant differences between Asacol MR and Octasa MR?’ it was clearly stated that ‘Octasa MR has not been compared directly in a clinical study with Asacol MR’. The Panel considered, however, that most readers would read the rest of the section and assume, even in the acknowledged absence of clinical data, that because the in vitro dissolution characteristics of Mesren and Asacol were similar, the clinical effects of Octasa MR and Asacol MR would also be similar. There was no clinical data to show that this was so. The Panel considered that the supplement was misleading in this regard. A breach of the Code was ruled.
Warner Chilcott noted that the y-axis of a graph was unlabelled and so it was unclear and ambiguous as to what was presented; it was impossible for the reader to interpret the findings presented. Warner Chilcott alleged that Tillotts had thus failed to maintain high standards in terms of representing the data and reviewing the article before publication.
The Panel noted that the graph was referenced to ‘Tillotts Pharma 2012. Data on file’ and headed ‘Dissolution of Mesren MR 400mg vs Asacol Mr 400mg and 800mg’. The y-axis was not labelled and so in that regard the Panel considered that the graph did not reflect the evidence clearly. The Panel ruled a breach of the Code. The Panel further considered that the use of a poorly labelled graph meant that high standards had not been maintained. A breach of the Code was ruled.
Warner Chilcott alleged that the figure presented for the annual cost of Asacol, 2.4g/day, should be £715.58 and not £715.40 as shown. This error meant that all data derived from this figure was also inaccurate.
Warner Chilcott further submitted that the table was misleading in that it failed to take into account possible changes of dose through a year as patients responded, or not, to therapy. Failure to take this into account in the costs therefore presented an artificial and misleading scenario that would not be encountered in clinical practice and therefore this table presented inflated and unrealistic cost savings that could never be achieved.
Warner Chilcott further submitted that the table failed to state that to obtain the proposed cost savings, the calculations assumed that all 300 patients (the typical number of patients with ulcerative colitis in an average primary care trust (PCT)) would be switched from Asacol to Octasa. This was simply not the case. Although Asacol was the market leader, it had only approximately 40% of market share. As this had not been taken into account, the figures proposed were inflated and misleading.
Other factors omitted from the calculations presented in the table were the cost of implementing such a switch and the management of any relapses or other adverse events. Warner Chilcott was not aware of any clinical study that could be used to accurately describe the true impact of such a switch programme in terms of cost savings or clinical benefit for the patient. However, Robinson et al (2013) demonstrated that stable, adherent patients prescribed Asacol MR formulations had a 3.5 times higher risk of experiencing a flare when switched to another mesalazine product compared with being maintained on Asacol.
The Panel noted that the table at issue compared the daily and annual costs of Octasa MR 400mg, Octasa MR 800mg and Asacol MR all at 2.4g/day and stated the annual cost savings per patient and per 300 patients if Octasa was prescribed instead of Asacol. The daily cost for Asacol was stated to be £1.96 with an annual cost of £715.40. The Panel noted that data from Tillotts showed that 120 Asacol MR 400mg tablets cost £39.21 ie 196.05 pence per dose of 2.4g which gave an annual cost of £715.58. The Panel noted that the table stated that the annual cost of Asacol 2.4g/day was £715.40 which was not so. The Panel considered that the table was not accurate in that regard as alleged and a breach of the Code was ruled.
The Panel noted that the table stated the annual cost savings per 300 patients if they were prescribed Octasa 2.4g/day instead of Asacol 2.4g/day. The authors had stated that 300 was the typical number of patients for an average PCT, based on a population of 300,000 and an estimated prevalence of ulcerative colitis of between 120 and 150 per 100,000. The Panel noted that this would therefore mean that an average PCT would have 360 to 450 ulcerative colitis patients.
The Panel noted that Tillotts had stated that the prevalence of ulcerative colitis was 240 per 100,000 population and so an average PCT with 350,000 people would have 840 ulcerative colitis patients. Ninety per cent of those patients would be on mesalazine (756) and at least half of them (378) would be on Asacol given its market share.
The Panel thus noted that the authors’ justification for assuming 300 patients and Tillotts’ justification for the same were quite different. In that regard the Panel considered that the assumptions made in the table were unclear and in that regard the comparisons made within the table were misleading and the data within the table could not be substantiated. Breaches of the Code were ruled.
The Panel noted that Robinson et al post-dated the preparation date of the educational update (December 2012). Robinson et al, however, was a retrospective study using a UK pharmacy dispensing database. Although the authors referred to a 3.5 times greater risk of relapse in adherent patients switched from one mesalazine product to another, compared with non-switch patients, the authors stated that further research was needed before making firm conclusions about the implications of the results for disease management. The Panel noted that there was no clinical data before it which showed that patients switched from one mesalazine to another were more likely to experience a flare in their condition as alleged. On that very narrow basis, the Panel considered that the data in table 1 was not misleading in that regard. No breach of the Code was ruled.
Warner Chilcott noted that the paragraph entitled, ‘Are there any cost differences?’ essentially summarised the data presented in table 1 and included claims that ‘Asacol MR is 50% more expensive than Mesren/Octasa MR 400mg and 25% more expensive than Octasa MR 800mg’ and that ‘One year of maintenance therapy (2.4g daily) would equate to a £72,000 difference in expenditure for 300 patients’. For all the reasons discussed above Warner Chilcott alleged that these claims were misleading, presented inaccurate and inappropriate cost comparisons and were incapable of substantiation.
The Panel noted that the section of the educational update at issue was a description and justification of the data used in the table considered above. Readers were referred to the table. The Panel noted its comments and rulings above and considered that they applied to the paragraph now at issue. Breaches of the Code were ruled.
Warner Chilcott noted that the concluding paragraph of the supplement contained the claim that ‘Octasa MR… represents the least expensive, pH-dependent, modified-release mesalazine product available in the UK’. As indicated above, even with a cost minimisation approach, which might be questionable with no head-to-head clinical data for any mesalazine vs Octasa, claims about the acquisition cost of mesalazine therapy should take into consideration the daily mesalazine dosage which varied by product and indication. Using the recommended dosing schedules and the prices presented in MIMS it was clear that there were mesalazine products/doses available in the UK with a lower acquisition cost than some daily doses of Octasa, including pH-dependent, modified release tablets. Thus, this claim was alleged to be inaccurate, misleading and incapable of substantiation.
The Panel noted its comments above and considered that they applied here. Breaches of the Code were ruled.
Warner Chilcott submitted that Tillotts’ close involvement in the writing, review and approval of this item and in the provision of data to the authors should have assured that the highest standards of content would be maintained. Instead there were a number of fundamental inaccuracies and breaches of the Code which collectively reflected failure to maintain high standards.
The Panel noted its rulings above of breaches of the Code and considered that high standards had not been maintained. A breach of the Code was ruled.
Warner Chilcott was concerned that the multiplicity of fundamental errors and breaches of the Code contained within the supplement potentially put ulcerative colitis patients at risk. A breach of Clause 2 was alleged.
The Panel noted its rulings above and that some of the matters considered overlapped. Although concerned about the poor standard of the material at issue, the Panel did not consider that it was such as to bring discredit upon, or reduce confidence in, the industry. No breach of Clause 2 was ruled.
Warner Chilcott UK Ltd complained about the promotion of Octasa (mesalazine modified- release tablets) by Tillotts Pharma UK Ltd. The material at issue was a journal supplement (ref UK/ OC/0001/0113) published in the British Journal of
Clinical Pharmacy. Tillotts submitted that it had already agreed to refrain from citing the journal supplement as a reference. The journal supplement had been used with health professionals involved in medicines budget management.
Warner Chilcott marketed Asacol (mesalazine modified release).
1 Disguised promotion
COMPLAINT
Warner Chilcott submitted that the supplement looked like a non-promotional, educational update – as indicated by its title ‘Educational update’ – produced by two independent health professionals and formatted in the house style of the British Journal of Clinical Pharmacy. These features were not consistent with the supplement being a promotional item. The Code was explicit on this point and clearly indicated that promotional material in journals should not resemble independent editorial matter. Warner Chilcott alleged a breach of Clause 12.1.
RESPONSE
Tillotts strongly disagreed that the educational update was disguised promotion.
Tillotts submitted that it did not pay for the authorship or publication of the educational update. Tillotts had not had editorial control over the content but had provided data and had been involved in the editorial process, which was clearly stated on the front cover and at the end of the update.
Although the educational update was not written as a promotional piece, it supported the use of Octasa and as such had been offered and provided by Tillotts to support the argument for using Octasa MR 400mg as a lower cost substitute for Asacol MR 400mg. This use of the educational update by Tillotts was promotional.
Tillotts aimed to adhere to the Code and so it ensured that its involvement was clearly and unambiguously stated in the declaration on the front cover; it provided a job bag number and prescribing information. These additions, in line with good practice, demonstrated Tillotts’ involvement and prevented the supplement being considered disguised promotion.
The house style layout and design used in the update was consistent with other articles recently published in the same journal. These articles bore a similar declaration. There was no intention to disguise this.
Tillotts noted that this document was an update to
Grosso et al (2009) published in the same journal. Tillotts was not involved in the production or compilation of the original article.
PANEL RULING
The Panel noted that it was acceptable for companies to sponsor material. It had previously been decided that the content would be subject to the Code if it was promotional in nature or if the company had used the material for a promotional purpose. Even
if neither of these applied, the company would be liable if it had been able to influence the content of the material in a manner favourable to its own interests. It was possible for a company to sponsor material which mentioned its own products and not be liable under the Code for its contents, but only if it had been a strictly arm’s length arrangement with no input by the company and no use by the company of the material for promotional purposes.
The journal supplement in question was written in conjunction with Tillotts; the company had provided data and reviewed and approved the article. The supplement was entitled ‘Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modified-release mesalazine formulation available?’. Prescribing information for Octasa was included on page 4 of the supplement. The Panel considered that Tillotts was inextricably linked to the production of the supplement, there was no arm’s length arrangement. Further, the company had submitted that it had provided reprints of the supplement to support its product, Octasa, vs Asacol and had cited it as a reference in materials. In the Panel’s view, Tillotts was thus responsible under the Code for the content of the supplement.
The front cover of the supplement was headed ‘Educational update’ which was underlined in red. The names of two independent authors appeared in the middle of the front cover. The outside top corner of each page of the article which made up the supplement, featured a red box labeled ‘Educational update’ in bold white type. The Panel noted that a declaration of sponsorship appeared at the bottom of the cover page and again at the end of the article on page 3; the prescribing information for Octasa appeared on page 4.
The Panel noted Tillotts’ involvement with the material and considered that although there were elements to show that the supplement was a promotional piece, its prominent characterisation as an ‘Educational update’ was such that the promotional nature of the material was disguised. In this regard, the Panel further noted Warner Chilcott’s submission that the supplement was formatted in the house style of the journal. Although the Panel had not been provided with a copy of The British Journal of Clinical Pharmacy, it noted that Grosso et al, previously published in the same journal, had a similar three column layout and heading structure. A breach of Clause 12.1 was ruled.
2 Declaration of sponsorship
COMPLAINT
Warner Chilcott acknowledged that a declaration of sponsorship was present, but considered that its font size was disproportionately small and the reader could easily miss it at the foot of the first page. Even if this declaration was read, claims for Octasa had already been made earlier on the page. The Code stated that the declaration of sponsorship must be sufficiently prominent to ensure that readers of sponsored material were aware of it at the outset. Given the size and location of the declaration,
Warner Chilcott alleged a breach of Clause 9.10.
RESPONSE
Tillotts disagreed. As stated above the declaration was clear and of appropriate prominence on the front cover and consistent with the publisher’s own standards for similar declarations in the same journal. In Tillotts’ view, the declaration highlighted its involvement and was not in breach of Clause 9.10.
Tillotts submitted that the declaration was appropriately sized, in a prominent position and occupied 20% of the cover depth and the full width. The declaration was in a clear font and of a size that could be read without difficulty under normal circumstances. The declaration stated:
‘This educational update was written in conjunction with Tillotts Pharmaceuticals. Tillotts Pharmaceuticals provided no funding to the authors for the creation of this article but have provided data and reviewed and approved the article. Final editorial control rested with the Journal. Prescribing information can be found on page 4. Date of preparation: December 2012 UK/OC/001/0113.’
In addition there was a clear acknowledgement on page 3 at the end of the educational update, in consistent text size with the body text of the update, that stated:
‘This educational update was written in conjunction with Tillotts Pharmaceuticals. Tillotts Pharmaceuticals provided no funding to the authors for the creation of this article but have provided data and reviewed and approved the article. Final editorial control rested with the Journal.’
Tillotts submitted that this reiterated its involvement. Therefore there were clear declarations, at both the start and the end of the educational update. Tillotts denied a breach of Clause 9.10.
PANEL RULING
The Panel noted that Clause 9.10 required companies to include a declaration of sponsorship on, inter alia, all materials relating to medicines and their uses. The supplementary information stated that the declaration of sponsorship must be sufficiently prominent to ensure that readers of sponsored material were aware of it at the outset.
The Panel noted that Tillotts’ declaration of sponsorship appeared on the front cover of the supplement and again at the end of the article. The declaration on the front cover was at the bottom of the page in small white type (a lower case ‘m’ was less than 2mm high) on a dark grey background. The dark grey band at the bottom of the page occupied 22% of the cover depth; the declaration of sponsorship statement within that band only occupied 5% of the cover depth, not 20% of it as submitted by Tillotts. The declaration statement was below larger type, on the same dark grey background, which referred to the associated journal. All other text on the cover was similarly in bigger and/or bolder type. The prominence of the heading ‘Educational update’, the title of the article and the author’s names and affiliations was emphasized by the bold white type
in which they were written appearing on a black background. The red underlining of ‘Educational update’ kept the reader’s eye to the top or middle of the page. In the Panel’s view, the declaration of sponsorship was such that the reader’s eye would not be drawn to what appeared to be ‘the small print’ at the bottom of the page. In that regard the Panel did not consider that the statement was sufficiently prominent to ensure that readers were aware of it at the outset. A breach of Clause 9.10 was ruled.
3 Claim ‘Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modified-release mesalazine formulation available?’
This claim appeared as the title of the supplement and of the article.
COMPLAINT
Warner Chilcott noted the question mark at the end of the title but considered that this did not alter the nature of this wording, ie it was a claim for Octasa MR. Although no direct attempt to substantiate this claim was made, the reader was introduced in the first paragraph of the article to a list of available modified-release mesalazine products. No cost data were presented for these products yet the title implied that Octasa was the cheapest option available in this list of seven products.
However, even if taking a cost minimisation approach, which might be questionable with no head-to-head clinical data for any of these products vs Octasa, the acquisition cost of mesalazine therapy should also take into consideration the prescribed daily dosage of mesalazine which varied by product and indication. Using the recommended dosing schedules and the prices presented in MIMS, May 2013, it was clear that there were mesalazine products/doses available in the UK with a lower acquisition cost than some daily doses of Octasa, including pH-dependent, modified release tablets.
Furthermore, this claim implied that both Octasa preparations were equivalently priced, which was not so. Indeed, as shown in table 1 of the item, the daily cost of 2.4g/day mesalazine was greater for Octasa MR 800mg tablets than for Octasa MR 400mg tablets. Clearly both Octasa products could not be the lowest cost formulation available as one was more expensive than the other. Thus, to make a broad claim that Octasa MR was the lowest cost, oral, pH-dependent, modified-release mesalazine formulation available was inaccurate, misleading and incapable of substantiation and in breach of Clauses 7.2 and 7.4.
RESPONSE
Tillotts disagreed that the educational update was in breach of Clauses 7.2 and 7.4 of the Code. The information, claims and comparisons were accurate and not misleading, and could be substantiated.
The question mark in the title clarified the purpose of the preceding words and raised debate around the topic. Questions were intended to raise debate and discussion. It was a question both pertinent to the timing of the publication, and relevant to the content of the educational update. The update set out to answer the question.
As stated to Warner Chilcott, Octasa was the lowest cost, pH-dependent formulation dose-for- dose. Tillotts was unsure why Warner Chilcott deemed this not to be the case and would have welcomed further communication on the matter.
Tillotts noted that under the European Medicines Evaluation Agency (EMEA) guidelines for production of generic medicines, two medicines which contained the same active substance were considered bioequivalent if they were pharmaceutically equivalent or pharmaceutical alternatives and their bioavailabilities (rate and extent) after administration in the same molar dose lay within acceptable predefined limits. These limits were set to ensure comparable in vivo performance, ie similarity in terms of safety and efficacy.
Tillotts noted that the Asacol patent expired in 2002, since then there had been a generic alternative (Mesren). The original application was submitted by Norton Healthcare to the Medicines and Healthcare Products Regulatory Agency (MHRA) for approval of Mesren MR 400mg tablets. This was a bibliographical application (art 4.8(a)(ii) of Directive 65/65/EC as amended), which permitted the applicant to refer to published scientific literature to show that the constituents of the medicine had a wellestablished medicinal use with recognized efficacy, and an acceptable level of safety. There was no requirement to include the results of clinical trials in accordance with the second paragraph of Article 1 of Directive 75/318/EEC. Therefore, a direct headto-head efficacy study between the innovator and generic product was not required.
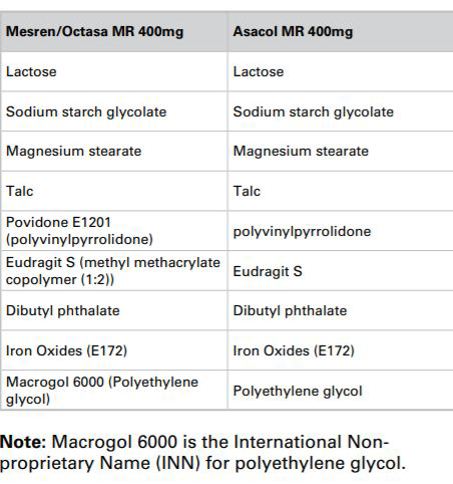
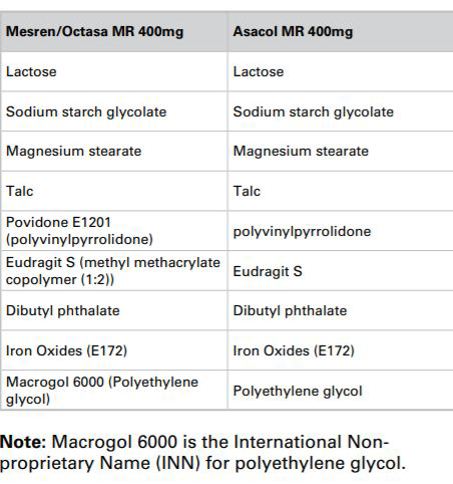
Both Asacol MR 400mg and Mesren/Octasa MR 400mg contained the same amount of mesalazine and shared the same excipients. Specific differences in terminology and nomenclature were due to the differences in the regulatory bodies (EU for Mesren/ Octasa and Food and Drug Administration (FDA) for Asacol).
Following MHRA grant to Norton, the licence for Mesren MR 400mg tablets was transferred to Teva and then to Tillotts. The regulatory requirements of the change of ownership required only the data which controlled the manufacture of the medicine to be transferred from Norton to Teva, and then Teva to Tillotts. The name of ‘Mesren MR 400mg Tablets’ was then changed to ‘Octasa 400mg MR Tablets’ by a variation.
Tillotts submitted that the MHRA was satisfied that head-to-head trials of Asacol and Mesren/Octasa were not required. Sufficient data existed to satisfy the licensing authority that there was comparable safety and efficacy. There was no scientific reason why a patient on Asacol would require a greater or lesser dose of Octasa. It was completely reasonable to forecast that a patient on Asacol would transfer to the same dose and strength of Octasa. As all strengths of Octasa had a lower acquisition price than the comparable Asacol preparations it followed that switching patients from Asacol to Octasa would reduce medicines expenditure in the NHS. Under any analysis, Octasa branded mesalazines were lower in cost than Asacol. Comparing costs between 400mg and 800mg tablets did not alter this fact; a patient on 2.4g of the more expensive Octasa 800mg would cost the NHS less than a patient on 2.4g of Asacol MR 400mg.
Tillotts submitted that Warner Chilcott was misguided in its calculations and for the reasons above Tillotts was not in breach of Clauses 7.2 and 7.4.
In response to a request for further information, Tillotts provided a table of data which showed all of the available mesalazine formulations and used July 2013 MIMS as the data source (Tillotts submitted that the NHS Tariff prices had not changed between March and August 2013).
Tillotts submitted that the data showed:
- The daily cost of acute and maintenance treatments within the licensed dosage range for adults treated with mesalazines
- Octasa 400mg had the lowest daily maintenance treatment cost for all mesalazines (the most frequently prescribed dose) and the lowest annualized treatment cost
- In practical terms Octasa MR 400mg was also the lowest cost acute phase treatment.
Tillotts stated that the educational update specifically focused on Asacol, Mesren, Octasa and Ipocol, all of which were pH-dependent 400mg tablets with comparable release profiles and dosage range. When the focus was on these comparable treatments the data conclusively supported the claim that Octasa 400mg was the lowest cost pH-dependent mesalazine.
Tillotts added that when high strength pH-dependent formulations were compared as a separate subcategory, Octasa MR 800mg was also the lowest cost when comparable daily doses were examined.
PANEL RULING
The Panel noted that the journal supplement was entitled ‘Introducing Octasa MR (mesalazine) – The lowest cost, oral, pH-dependent, modified-release mesalazine formulation available?’. In the Panel’s view, although the title was presented as a question, readers would assume it was a claim ie that Octasa MR was the lowest cost, oral, pH-dependent, modified-release mesalazine available.
The first paragraph of the article introduced the reader to the seven modified-release mesalazine preparations which were available until the end of 2012 ie Asacol MR, Ipocol, Mesren MR, Mezavant XL,
Pentasa, Salofalk and Octasa MR. In that regard the Panel considered that the claim would be seen in the context of these seven medicines ie that Octasa was the lowest cost compared with them all. The Panel noted that the additional data provided by Tillotts detailed the cost of all of the mesalazine products currently available (ie the seven listed above minus Mesren which had been discontinued). With regard to acute treatment with mesalazine, the data provided by Tillotts showed that Octasa MR 400mg tablets (2.4g/day) was the least expensive treatment option. However, for maintenance therapy a dose of Salofalk 1.5g was the least expensive option and Pentasa sachets were also less expensive than Octasa given that the highest maintenance dose of Octasa was 2.4g/day.
The Panel considered that the basis of the claim at issue had not been made abundantly clear in the journal supplement. It was not clear as to which doses were included in the comparison and if the claim related to acute treatment, maintenance treatment or both. The Panel considered that the claim was misleading as alleged. A breach of Clause 7.2 was ruled. The Panel considered that the claim could not be substantiated. A breach of Clause 7.4 was ruled.
4 Statement ‘This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care’.
This statement appeared as part of the sub-heading to page 1 of the article.
COMPLAINT
Warner Chilcott stated that in its view, the article neither presented nor referred to any evidence or data relating to the clinical benefits of Octasa in patient care. The supplement discussed the in vitro dissolution characteristics and cost differences between Asacol MR 400mg/800mg tablets and Octasa (Mesren) MR 400mg/800mg tablets. It appeared therefore that the statement ‘without compromising patient care’ was based purely on the extrapolation of in vitro data to the clinical situation and implied that without clinical evidence, the products discussed could be simply interchanged without affecting patient management or compromising patient care. To make this assumption without clinical data to show that it was of direct relevance and significance was misleading, in breach of Clause 7.2.
RESPONSE
Tillotts submitted that Warner Chilcott had taken the statement out of the context of the article to create a complaint. The article actually stated ‘The discontinuation of Mesren MR (mesalazine; Teva Pharmaceuticals) could have considerable cost implications for the NHS. This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care’. As explained above, Octasa MR 400mg was Mesren rebranded following the transfer of the marketing authorization to Tillotts. Therefore it could be fairly assumed that keeping patients on exactly the same formulation/medicine would not compromise care.
Tillotts submitted that Warner Chilcott wanted to transfer patients from Mesren to Asacol as demonstrated in its recent advertising. The allegation of a breach of Clause 7.2 was unsupportable on the basis that Octasa MR 400mg, and Mesren MR 400mg contained exactly the same active ingredient, excipients and had the same coating and release profile (they were the same product with a change of name). These medicines were interchangeable.
There was over 10 years of experience with Mesren in the UK. A proportion of these patients were initiated on Asacol in secondary care and transferred in primary care to Mesren. There was no evidence that transferring patients from Asacol to Mesren caused any additional risk to the patients’ health.
Tillotts reiterated that Norton Healthcare was originally granted a licence for the product in 2002, this was transferred to Teva (when Teva acquired Norton Healthcare) and subsequently, in 2012, the licence was transferred to Tillotts. The transfer of the licence to Tillotts also included a brand name change from Mesren to Octasa. It was clear therefore that all patients who had previously taken Mesren should be transferred to Octasa as it was the same medicine and in doing so the cost to the NHS would be kept down, because there would be 50% increase in costs to the NHS if these patients migrated to Asacol.
Tillotts denied a breach of Clause 7.2.
PANEL RULING
The Panel noted that the statement at issue was the second sentence to the subheading on page 1 of the article. The sub-heading, in full, read:
‘The discontinuation of Mesren MR (mesalazine’ Teva Pharmaceuticals) could have considerable cost implications for the NHS. This article describes how the launch of Octasa MR (Tillotts Pharmaceuticals) provides an opportunity to keep costs down without compromising patient care.’
The Panel noted that with the discontinuation of Mesren, patients previously taking that medicine would have to be switched to an alternative mesalazine product. The Panel further noted that Octasa was, as stated in the article, essentially a rebrand of Mesren; the formulation of both medicines was the same. In the Panel’s view, patients switching from Mesren to Octasa should not notice a clinical difference in therapy.
The Panel considered that in the context of the discontinuation of Mesren MR, the statement at issue was not misleading as alleged. No breach of Clause 7.2 was ruled.
5 Disregard of current guidelines and recommendations on prescribing modified- release mesalazine
COMPLAINT
Warner Chilcott submitted that whilst the supplement referred to the British Society of Gastroenterology (BSG), the European Crohn’s and Colitis Organisation (ECCO) and the British National Formulary (BNF) guidelines and statements, it was quick to disregard the caution represented by these respected national and international bodies in relation to indiscriminate switching between mesalazine brands and the recommendation to prescribe modified-release mesalazine by brand. To date, there had been no head-to-head clinical studies between Octasa and any other mesalazine and very few head-to-head clinical studies between the different modified-release mesalazines in general. Absence of evidence showing clinical differences between mesalazines (because these studies had not been conducted) was not equivalent to evidence demonstrating no clinically significant differences between the mesalazines, hence the appropriate caution in the guidelines that these products should not be considered interchangeable. To dismiss these cautions and recommendations clearly supported Tillotts’ promotional drive to have patients receiving other mesalazines indiscriminately switched to Octasa. Dismissal and misrepresentation of the guidelines in this way was misleading and did not encourage the rational use of Octasa.
Furthermore, Warner Chilcott noted the comment that the BNF statement was ‘originally made before the introduction of Mesren MR 400mg and Octasa MR 400mg to the UK market’. Whilst that might or might not be true (Mesren MR 400mg tablets were first licensed in the UK in November 2003) the comment implied that the BNF’s position was outdated and could be further disregarded on these grounds. Warner Chilcott noted that the hard copy BNF was updated every six months and the digital version, every month. As the BNF continued to use this statement, it presumably reflected the BNF’s current position and was not an outdated recommendation as implied.
Warner Chilcott alleged that this section of the supplement misled by distortion and failed to encourage the rational use of Octasa, in breach of Clauses 7.2 and 7.10.
RESPONSE
Tillotts strongly disagreed that the educational update breached Clauses 7.2 or 7.10. The company considered that the information provided was not misleading and that it did encourage the rational use of medicines.
Tillotts stated that the basis of the complaint was unclear. The educational update provided balanced, fair and rational evaluations of medicines that shared the same active ingredient, the same excipients and the same delivery profile; it did not advocate indiscriminate switching. The article specifically stated, ‘This review will focus on Mesren MR 400mg, Octasa MR 400mg and Asacol MR 400mg, since other modified-release mesalazine preparations have marked differences in delivery characteristics’, the review was therefore very discriminate and was focused entirely on these three medicines which, as already established, shared the same delivery profiles, delivery systems, excipients and active ingredients. As stated in inter-company dialogue, none of the guidelines referred to by Warner Chilcott made such a caution in relation to ‘indiscriminate’ switching.
The BSG and ECCO guidelines were accurately quoted within the educational update. The reader was alerted to these guidelines and relevant extracts quoted from these respected guidelines. The article did not disregard the guidelines but firmly supported their recommendations. The educational update also quoted the BNF guidance ‘The delivery characteristics of oral mesalazine preparations may vary; these preparations should not be considered interchangeable’. In the case of Mesren/Octasa MR 400mg and Asacol MR 400mg the delivery characteristics did not vary, this was specifically discussed and demonstrated by the two graphs showing comparative dissolution profiles. The article specifically asked the reader to consider very discriminate brand switching in alignment with the established guidelines. Further, it was the purpose of this type of journal to challenge readers to update their own knowledge and consider whether guidance that their organizations currently provided was fully informed such as including cost as one of their decision-making criteria when considering oral, pHdependent mesalazine.
The educational update stated that the BNF guidelines were written before Mesren was introduced, this was factually correct. The BNF guidance had not changed since it was introduced, despite new brands entering the market, however as stated above its intention was to guide prescribers away from switching patients between mesalazines with differing delivery characteristics, unlike Mesren/ Octasa MR 400mg and Asacol MR 400mg which shared the same dissolution profiles and therefore delivery characteristics.
PANEL RULING
The Panel noted that the first section of the journal supplement introduced the reader to seven modified release mesalazine preparations and then stated that the article would describe some of the similarities and differences of three of them – Mesren, Octasa and Asacol. The next section of the article referred to prescribing guidelines and that the BSG and ECCO had recommended that modified-release mesalazine should be prescribed by brand. It was stated however, that both guidelines appeared to suggest that there was little in the way of significant differences between available products with regard to important clinical outcomes. It was noted that the BNF statement which advised that oral mesalazine preparations should not be considered interchangeable was made before Mesren and Octasa had been introduced to the UK market.
The Panel considered that overall, the take home message was that it was not important to prescribe any modified-release mesalazine by brand and that they were all essentially interchangeable. In that regard the Panel noted that the sub-heading referred to ‘modified release mesalazine’ and so it appeared that the subsequent discussion was not restricted in its scope to Asacol, Mesren and Octasa. The Panel considered that this was misleading. A breach of Clause 7.2 was ruled. The Panel did not consider that the information encouraged the rational use of Octasa. A breach of Clause 7.10 was ruled.
6 Paragraph entitled ‘Are there any significant differences between Asacol MR and Octasa MR?’
COMPLAINT
Warner Chilcott noted that although the supplement conceded that Octasa had not been compared directly with Asacol MR in a clinical setting, no clinical efficacy or safety data for either Octasa or Asacol was presented. Clearly, the consideration of clinical evidence should be fundamental to any comparative evaluation of two products. Instead, the article focussed on data from in vitro dissolution studies to make a case for (clinical) similarity between Asacol and Octasa.
However, the methodology of these in vitro studies made it impossible to draw any meaningful conclusions about the similarities or differences between these products in vivo, let alone in various stages of disease activity in patients with ulcerative colitis. Presenting dissolution data in isolation was problematic, as in vitro dissolution studies could not fully reproduce the conditions of the gastrointestinal tract in patients with ulcerative colitis. Furthermore, no statistical comparisons between the findings for Mesren and Asacol were presented and no in vitro/in vivo correlation had been established to indicate the potential clinical significance of the findings. Warner Chilcott noted that Fadda and Basit (2005), presented in the supplement even commented on the poor in vitro/in vivo correlations obtained for pH-responsive, modified-release dosage forms. Thus, any conclusions about the significance of the findings of these in vitro data were impossible and attempting to do so in this manner alleged to be misleading in breach of Clause 7.2.
RESPONSE
Tillotts submitted that as already stated, Mesren/Octasa MR 400mg was a generic copy of Asacol MR 400mg which lost its patent protection in 2002. Tillotts was the originator of Asacol MR and continued to manufacture and distribute 400mg modified-release mesalazine in 55 countries worldwide with over 1.5 million patients-years’ experience with this formulation, showing that it was well tolerated and effective. Warner Chilcott currently manufactured Asacol MR 400mg to the same formulation as that originally developed and marketed by Tillotts in the UK. This same formulation was used by Tillotts to manufacture Octasa MR 400mg in the UK (Tillotts noted that in the UK the brand name Asacol was the commercial property of Warner Chilcott). Tillotts however continued to manufacture and market its mesalazine product as Asacol MR 400mg for markets outside the UK. The question asked by the authors was completely valid.
Tillotts submitted that head-to-head studies were deemed unnecessary by the MHRA when Mesren was approved, as Mesren (Octasa MR 400mg) and Asacol MR 400mg were pharmaceutically equivalent. Dissolution data presented to pharmacists familiar with these analyses, supported this point, and showed no significant differences in dissolution.
Tillotts denied a breach of Clause 7.2.
PANEL RULING
The Panel noted that in the section of the supplement entitled ‘Are there any significant differences between Asacol MR and Octasa MR?’ it was clearly stated that ‘Octasa MR has not been compared directly in a clinical study with Asacol MR’. The relevant section reported that Fadda and Basit had shown that Mesren and Asacol had similar dissolution profiles and that a more recent study carried out by Tillotts showed very little difference in the dissolution profiles of the two products.
The Panel noted that the section at issue focussed on in vitro dissolution data. The supplementary information to Clause 7.2 of the Code stated that care should be taken with the use of in vitro data and the like so as not to mislead as to its significance. The extrapolation of such data to the clinical situation should only be made where there is data to show that it is of direct relevance and significance.
The Panel noted that the first sentence of the section at issue stated that there had been no clinical comparison of Asacol MR and Octasa MR. The Panel further considered that most readers would read the rest of the section and assume, even in the acknowledged absence of clinical data, that because the in vitro dissolution characteristics of Mesren and Asacol were similar, the clinical effects of Octasa MR and Asacol MR would also be similar. There was no clinical data to show that this was so. The Panel considered that the supplement was misleading in this regard. A breach of Clause 7.2 was ruled.
7 Graph not fully labelled
COMPLAINT
Warner Chilcott noted that the y-axis of the graph at figure 2 was unlabelled and so it was unclear and ambiguous as to what was presented. Failing to label the graph made it impossible for the reader to interpret the findings presented. As this graph represented data on file provided by Tillotts, Warner Chilcott alleged that Tillotts had thus failed to maintain high standards in terms of representing its own data and reviewing the article before publication in breach of Clauses 7.2 and 9.1.
RESPONSE
Tillotts acknowledged that the y-axis was not labelled on figure 2: ‘Dissolution of Mesren MR 400mg vs Asacol MR 400mg and 800mg’, but denied a breach of Clauses 7.2 and 9.1.
Tillotts submitted that figures 1 and 2 were laid out side by side and the label of the y-axis of figure 1 could be applied to both graphs. The pages faced each other and readers were able to read across the page to review the two graphs side by side. However in order to increase the clarity of this item Tillotts submitted that it had contacted the editor of the British Journal of Clinical Pharmacy and suggested that a label be added to the y-axis of figure 2. Tillotts had also withdrawn reprints of the article from use and would only use them again if and when the omission was corrected.
Tillotts did not consider that the omission of the label rendered the figure misleading and it therefore denied a breach of Clause 7.2.
Tillotts also did not consider that the omission constituted a breach of Clause 9.1. Any potential reduction in clarity from this single omission was minor and was not misleading. It therefore did not represent a failure to maintain high standards of the order of magnitude referred to in the Code (eg causing offence).
PANEL RULING
The Panel noted that the graph was referenced to ‘Tillotts Pharma 2012. Data on file’ and headed ‘Dissolution of Mesren MR 400mg vs Asacol Mr 400mg and 800mg’. The y-axis was not labelled and so in that regard the Panel considered that the graph did not reflect the evidence clearly. In the Panel’s view it was immaterial that the graph was next to another similar graph which did have the y-axis labelled; each graph should be capable of standing alone. The Panel ruled a breach of Clause 7.2. The Panel further considered that the use of a poorly labelled graph meant that high standards had not been maintained. A breach of Clause 9.1 was ruled.
8 Cost comparison data
COMPLAINT
Warner Chilcott alleged that the figure presented for the annual cost of Asacol, 2.4g/day, should be £715.58 and not £715.40 as shown. This error meant that all data presented in rows three and four of the table (which included the incorrect figure for Asacol in its calculation) were also inaccurate. Warner Chilcott alleged a breach of Clause 7.2.
Warner Chilcott further submitted that the table was misleading in that if a patient failed to respond to Asacol or Octasa at a dose of 2.4g/day they would not be maintained on that dose for 365 days of the year; the dose would either be increased to 4.8g/ day in the case of patients with moderately active ulcerative colitis until symptoms were brought under control (typically 6-8 weeks) or be prescribed other medicines such as corticosteroids. Further, if patients responded to treatment with 2.4g/day, once symptoms were quiescent the dose of Asacol/Octasa was likely to be reduced for the maintenance of remission of ulcerative colitis. Failure to take this into account in the costs therefore presented an artificial and misleading scenario that would not be encountered in clinical practice and therefore this table presented inflated and unrealistic cost savings that could never be achieved.
Warner Chilcott further submitted that the table failed to inform the reader that to obtain the proposed cost savings, the calculations assumed that all 300 patients (the typical number of patients with ulcerative colitis in an average primary care trust (PCT)) would be switched from Asacol to Octasa. This was simply not the case. Even though Asacol was the acknowledged market leader, it had only approximately 40% of market share. As this had not been taken into account, the figures proposed were additionally inflated and misleading.
Other factors omitted from the calculations presented in table 1 were the cost of implementing such a switch and the management of any negative clinical impacts that the switch might have e.g. risk of relapse or other adverse event. Warner Chilcott was not aware of any clinical study that could be used to accurately describe the true impact of such a switch programme in terms of cost savings or clinical benefit for the patient. However, the potential impact of switching stable adherent patients between formulations was considered by Robinson et al (2013) who demonstrated that stable adherent patients prescribed Asacol MR formulations had a 3.5 times higher risk of experiencing a flare when switched to another mesalazine product compared with being maintained on Asacol.
Warner Chilcott therefore alleged that table 1 was misleading, presented inaccurate and inappropriate cost comparisons and was not capable of substantiation in breach of Clauses 7.2, 7.3 and 7.4.
RESPONSE
Tillotts strongly disagreed that the educational update breached Clauses 7.2, 7.3 and 7.4; the information provided and comparisons made were not misleading and could be substantiated.
Tillotts submitted that the assumptions used in the calculations were clearly stated. Warner Chilcott considered that the authors’ calculations were inaccurate in that the annual cost of Asacol should be £715.58 rather than £715.40 as stated (a difference of 18 pence). Tillotts was unsure as to how Warner Chilcott got to its figure as the stated daily cost of Asacol was £1.96 based on 2.4g/day. If this cost was multiplied by 365 days (as stated in the table) then the annual cost was £715.40 as stated ie £1.96 x 365 = £715.40. Tillotts stated that it would have welcomed further discussions with Warner Chilcott if it had raised this difference.
Tillotts stated that all assumptions used in the calculations had been clearly stated by the authors. For the purposes of health economic modelling and forecasting certain assumptions had to be made, in the educational update a fair assumption was made that the number of patients on less than 2.4g/ day would be counter balanced by the number of patients on more than 2.4g/day, as patients might increase their dose to 4.8g/day during a flare of ulcerative colitis. Approximately 70% of patients with ulcerative colitis who took mesalazines remained in remission each year, patients who relapsed might be treated by doubling the dose to 4.8g/day, which would double the cost. Whereas, if patients took 1.6g/day this would reduce the cost by 33%. A mean of 2.4g/day (which was clearly stated) was a fair and reasonable assumption on which to model. This was not misleading and therefore not in breach of Clause 7.2, 7.3 or 7.4.
The figures shown in table 1 were transparent. The difference in cost between 365 days’ treatment with Asacol vs Octasa was a cost reduction of £240.90/ patient treated with Octasa, which for 300 patients would amount to £72,270. The difference in cost between patients taking 2.4g/day of Asacol 400 vs Octasa 800 was lower at a daily difference of £1.58 and annualized in 300 patients to £41,244.
A population of 300 patients on Asacol was selected as typical for a PCT on the basis that ulcerative colitis had a prevalence of approximately 240 per 100,000 of the population in the UK (NICE CG166 guidelines). A typical PCT had a population of around 350,000, hence it would typically have 840 ulcerative colitis patients. The vast majority of these patients would be treated with a mesalazine first line, they might or might not have steroids and/or other topical forms of mesalazine included in their treatment regimens. However, it was assumed that the ‘other therapies’ remained constant and were not affected. The figures discussed in the educational update were the costs of treating patients with Asacol or Octasa only. If 90% of the treated population were on a mesalazine (which was a fair assumption), 756 patients would be on an oral mesalazine.
When the educational update was published, Asacol had a market share in excess of 50% (IMS RSA data December 2012 51.17%), this would be approximately 378 patients per typical PCT. This meant that the estimates which were discussed in the educational update were conservative.
Tillotts noted Warner Chilcott’s suggestion that switching patients might cause patient to flare but stated that there was no trial evidence to support this statement.
The cost savings achieved by Surrey PCT and discussed in the educational update had been realized through a programme managed by the author, a medicines management pharmacist with that PCT.
PANEL RULING
The Panel noted that the table at issue compared the daily and annual costs of Octasa MR 400mg, Octasa MR 800mg and Asacol MR all at 2.4g/day and stated the annual cost savings per patient and per 300 patients if Octasa was prescribed instead of Asacol. The daily cost for Asacol was stated to be £1.96 with an annual cost of £715.40. The Panel noted that data from Tillotts showed that 120 Asacol MR 400mg tablets cost £39.21 ie 196.05 pence per dose of 2.4g which gave an annual cost of £715.58. The Panel noted that the table stated that the annual cost of Asacol 2.4g/day was £715.40 which was not so. The Panel considered that the table was not accurate in that regard as alleged and a breach of Clause 7.2 was ruled.
The Panel noted that the table stated the annual cost savings per 300 patients if they were prescribed Octasa 2.4g/day instead of Asacol 2.4g/day. The authors had stated that 300 was the typical number of patients for an average PCT, based on a population of 300,000 and an estimated prevalence of ulcerative colitis of between 120 and 150 per 100,000. The Panel noted that this would therefore mean that an average PCT would have 360 to 450 ulcerative colitis patients.
The Panel noted that Tillotts had stated that the prevalence of ulcerative colitis was 240 per 100,000 population and so an average PCT with 350,000 people would have 840 ulcerative colitis patients. Ninety per cent of those patients would be on mesalazine (756) and at least half of them (378) would be on Asacol given its market share.
The Panel thus noted that the authors’ justification for assuming 300 patients and Tillotts’ justification for the same were quite different. In that regard the Panel did not consider that the assumptions made in the table were clear and in that regard the comparisons made within the table were misleading in breach of Clauses 7.2 and 7.3. The Panel considered that the data within the table could not be substantiated. A breach of Clause 7.4 was ruled. The Panel noted that Robinson et al post-dated the preparation date of the educational update (December 2012). Robinson et al, however, was a retrospective study using a UK pharmacy dispensing database. Although the authors referred to a 3.5 times greater risk of relapse in adherent patients switched from one mesalazine product to another, compared with non-switch patients, the authors stated that further research was needed before making firm conclusions about the implications of the results for disease management. The Panel noted that there was no clinical data before it which showed that patients switched from one mesalazine to another were more likely to experience a flare in their condition as alleged. On that very narrow basis, the Panel considered that the data in table 1 was not misleading in that regard. No breach of Clause 7.2 was ruled.
9 Paragraph entitled, ‘Are there any cost differences?’
COMPLAINT
Warner Chilcott submitted that this paragraph essentially summarised the data presented in table 1 and included claims that ‘Asacol MR is 50% more expensive than Mesren/Octasa MR 400mg and 25% more expensive than Octasa MR 800mg’ and that ‘One year of maintenance therapy (2.4g daily) would equate to a £72,000 difference in expenditure for 300 patients’. For all the reasons discussed in Point 8 above Warner Chilcott alleged that these claims were misleading, presented inaccurate and inappropriate cost comparisons and were incapable of substantiation in breach of Clauses 7.2, 7.3 and 7.4.
RESPONSE
Tillotts disagreed for the reasons stated in Point 8 above.
PANEL RULING
The Panel noted that the section of the educational update at issue was a description and justification of the data used in table 1 considered at Point 8 above. Readers were referred to table 1. The Panel noted its comments and rulings above and considered that they applied to the paragraph now at issue. Breaches of Clauses 7.2, 7.3 and 7.4 were ruled.
10 ‘Octasa MR … represents the least expensive, pH-dependent, modified-release mesalazine product available in the UK’.
COMPLAINT
Warner Chilcott noted that the concluding paragraph of the supplement contained the claim that ‘Octasa MR… represents the least expensive, pH-dependent, modified-release mesalazine product available in the UK’. As indicated in Point 3 above, even with a cost minimisation approach, which might be questionable with no head-to-head clinical data for any other mesalazine vs Octasa, claims about the acquisition cost of mesalazine therapy should also take into consideration the daily dosage (which varied by product and indication) of mesalazine that the patient was prescribed. Using the recommended dosing schedules and the prices presented in MIMS it was clear that there were mesalazine products/ doses available in the UK with a lower acquisition cost than some daily doses of Octasa, including pH-dependent, modified-release tablets. Thus, this claim was alleged to be inaccurate, misleading and incapable of substantiation and in breach of Clauses 7.2 and 7.4.
RESPONSE
Tillotts strongly disagreed with the complaint and denied any breach of Clauses 7.2 or 7.4. The claim at issue was a statement of fact as addressed in the company’s response to Point 3.
The concluding paragraph discussed the brand name change from Mesren to Octasa. Mesren was considered the cheapest pH-dependent, modifiedrelease mesalazine product in the UK but given the name change this was now Octasa MR 400mg. The emphasis of the educational update was a comparison of like-for-like treatments, Mesren/Octasa and Asacol; if patients were switched between Asacol and Octasa there would be a 34% cost reduction for the NHS. Other non-pH-dependent mesalazines on a dose per dose comparison with Octasa MR 400mg were also more expensive than Octasa. Octasa MR 400mg was the lowest cost, oral, pH-dependent mesalazine dose-for-dose. It was unclear as to what Warner Chilcott believed was inaccurate or misleading about this. Tillotts regretted that there had been no opportunity for further inter-company dialogue which might have resolved this.
Head-to-head trials did not exist because Mesren/ Octasa was a generic copy of Asacol and headto-head studies were not required by the MHRA because the formulation of Octasa and Asacol was considered to be sufficiently the same as not to warrant such trials.
The data provided was not misleading and could be substantiated. Tillotts denied a breach of Clauses 7.2 or 7.4.
PANEL RULING
The Panel noted its comments at Point 3 above and considered that they applied here. As at Point 3, the Panel considered that the basis of the claim at issue had not been made abundantly clear. It was not clear as to which doses were included in the comparison and if the claim related to acute treatment, maintenance treatment or both. For maintenance therapy, two preparations were shown to be less expensive than Octasa MR. The Panel considered that the claim was misleading as alleged. A breach of Clause 7.2 was ruled. The Panel considered that the claim could not be substantiated. A breach of Clause 7.4 was ruled.
11 Failure to maintain high standards
COMPLAINT
Warner Chilcott submitted that Tillotts’ close involvement in the writing, review and approval of this promotional item and in the provision of data to the authors should have assured that the highest standards of content would be maintained. Instead the item included a number of fundamental inaccuracies and breaches of the Code which should have been identified and corrected by Tillotts during its review. These inaccuracies collectively reflected failure to maintain high standards in breach of Clause 9.1.
RESPONSE
Tillotts strongly disagreed. As stated above, the inaccuracies claimed by Warner Chilcott seem to relate to its calculations rather than the authors’.
The educational update was an independently written and published update produced in the house style of the British Journal of Clinical Pharmacy. The information included in the update was accurate (as mentioned in Point 8) and as such Tillotts denied a breach of Clause 9.1.
PANEL RULING
The Panel noted its rulings above of breaches of the Code and considered that high standards had not been maintained. A breach of Clause 9.1 was ruled.
COMPLAINT
Warner Chilcott stated that materials associated with the promotion of prescription only medicines must never be such as to bring discredit upon, or reduce confidence in, the pharmaceutical industry. Unfortunately, given the multiplicity of fundamental errors and breaches of the Code contained within the supplement, despite the close involvement of Tillotts in its review and approval, Warner Chilcott was concerned that patients with ulcerative colitis had potentially been put at risk by this item and therefore it alleged a breach of Clause 2.
Warner Chilcott also noted its concerns about the responses that were received via inter-company dialogue which further reduced its confidence in Tillotts’ understanding of the Code and resulted in referral of the matter to the PMCPA in order to secure a timely and appropriate conclusion of this matter, which the company considered might otherwise not have occurred.
RESPONSE
For the reasons given above, and the fact that there were no inaccuracies, Tillotts clearly disagreed with the complaint. Tillotts did not consider that the educational update breached the Code, brought discredit on the industry or undermined patient safety. The educational update was independently written by pharmacists with budgetary responsibilities, for other health professionals (predominantly pharmacists) with budget responsibilities. It raised the question as to whether the NHS should pay more for similar products.
PANEL RULING
The Panel noted its rulings above and that some of the matters considered overlapped. Although concerned about the poor standard of the material at issue, the Panel did not consider that it was such as to bring discredit upon, or reduce confidence in, the industry. No breach of Clause 2 was ruled.
Complaint received 17 June 2013
Case completed 10 September 2013